Data Analyzer
Data Analyzer
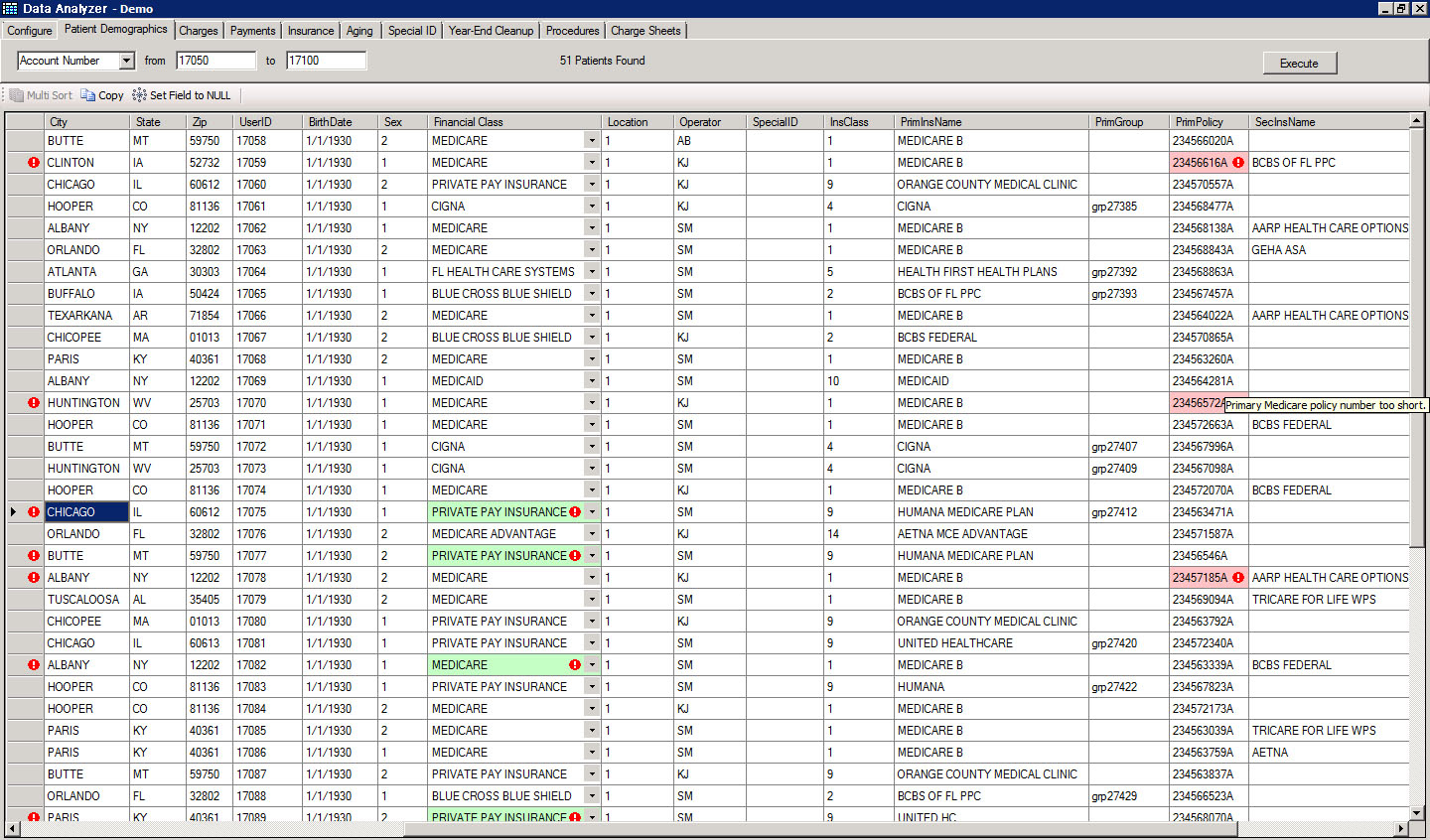
We have captured our 28 years of experience and intimate knowledge of the medical claims billing process into a rules engine that identifies potential red flags prior to submission of claims to a Clearing House. This allows us to correct, common and most not so common, causes of delayed payments, non-payments, under payments and no response class, before they go out.
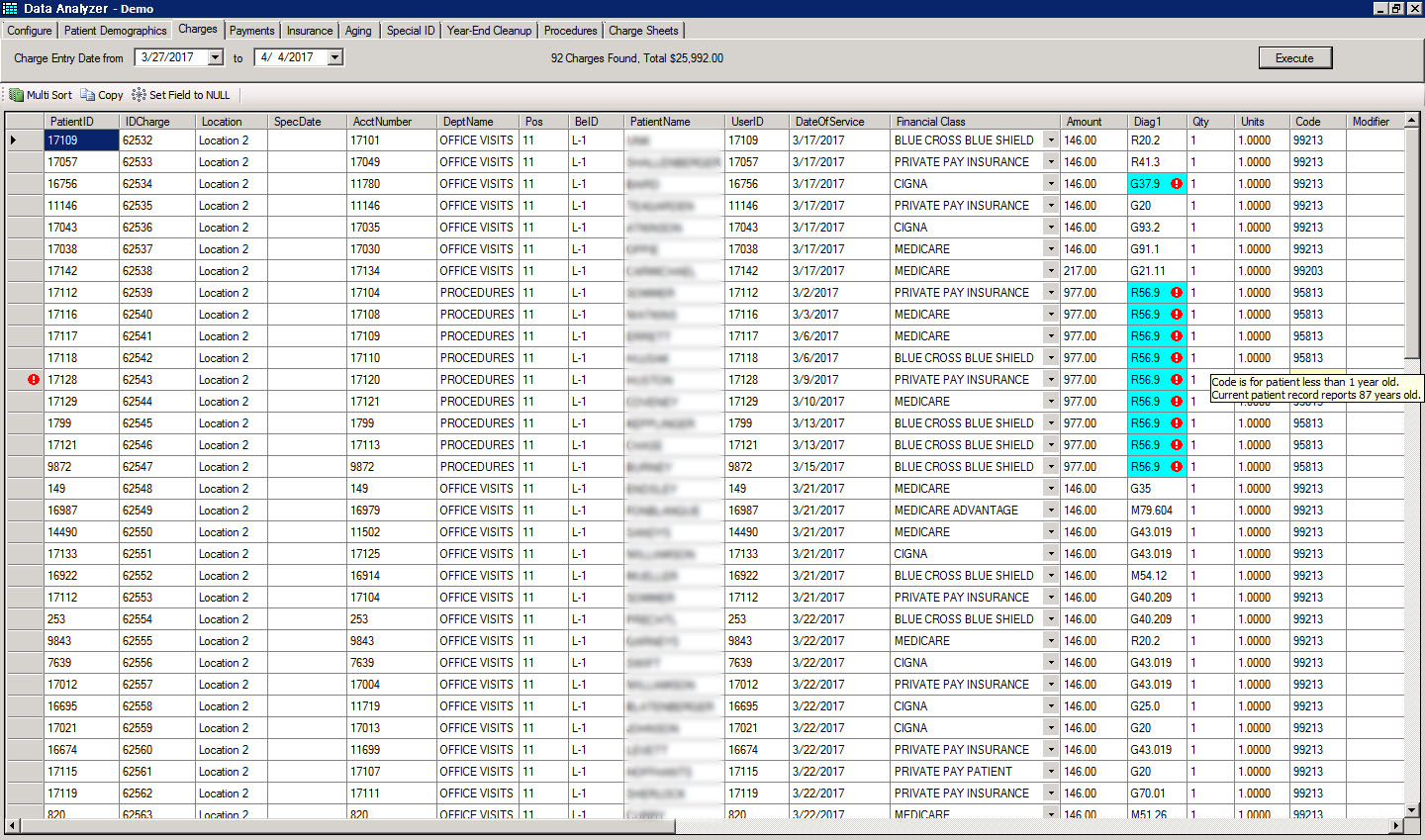
Our software displays errors and conflicts in an easy-to-review, Color-Coded Grid that results in efficient corrections and submissions. What is more, in some cases, the software is smart enough to recommend corrections, resulting in quick turn-around and submissions.
The rules of engagement, when it comes to maximizing revenue yield from medical claims, are constantly changing. The codes change, the rules on bundling change, and to make it more complicated, they vary with each Insurance Carrier. We stay on top of the game for our clients by constantly added to the hundreds of rules that we have generated. Furthermore, we evaluate each client’s payment patterns and add more rules that are specialty, location, carrier and practice specific. Billing services don’t get much more white glove than that.